Abstract
The need for stratification and a common scale amongst clinicians to evaluate and rate patients cognitive status has led to development of clinical scales and tests such as Mini-Mental Status Examination (MMSE) and Montreal Cognitive Assessment (MoCA)-as well as a dozen more tests. These test are administered mainly to detect Mild Cognitive Impairment (MCI) in older population, but in recent years their utility has increased in the realm of stroke care and research. Here, we argue that in clinical settings, despite their usefulness, these tests do not provide helpful information and potentially create a preconceived notion about patients cognitive status if administered in the first few weeks of stroke onset.
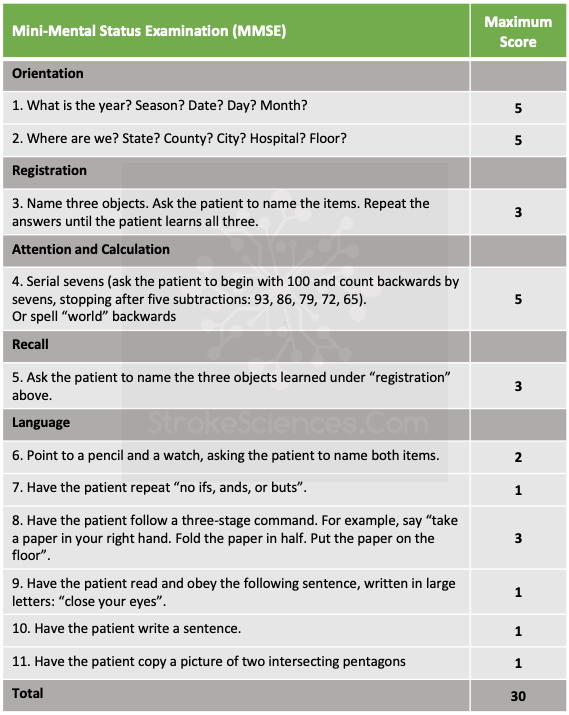
Table
- 1- Introduction
- 2- Mini-Mental Status Examination (MMSE): Sensitivity, Specificity and Predictive Values
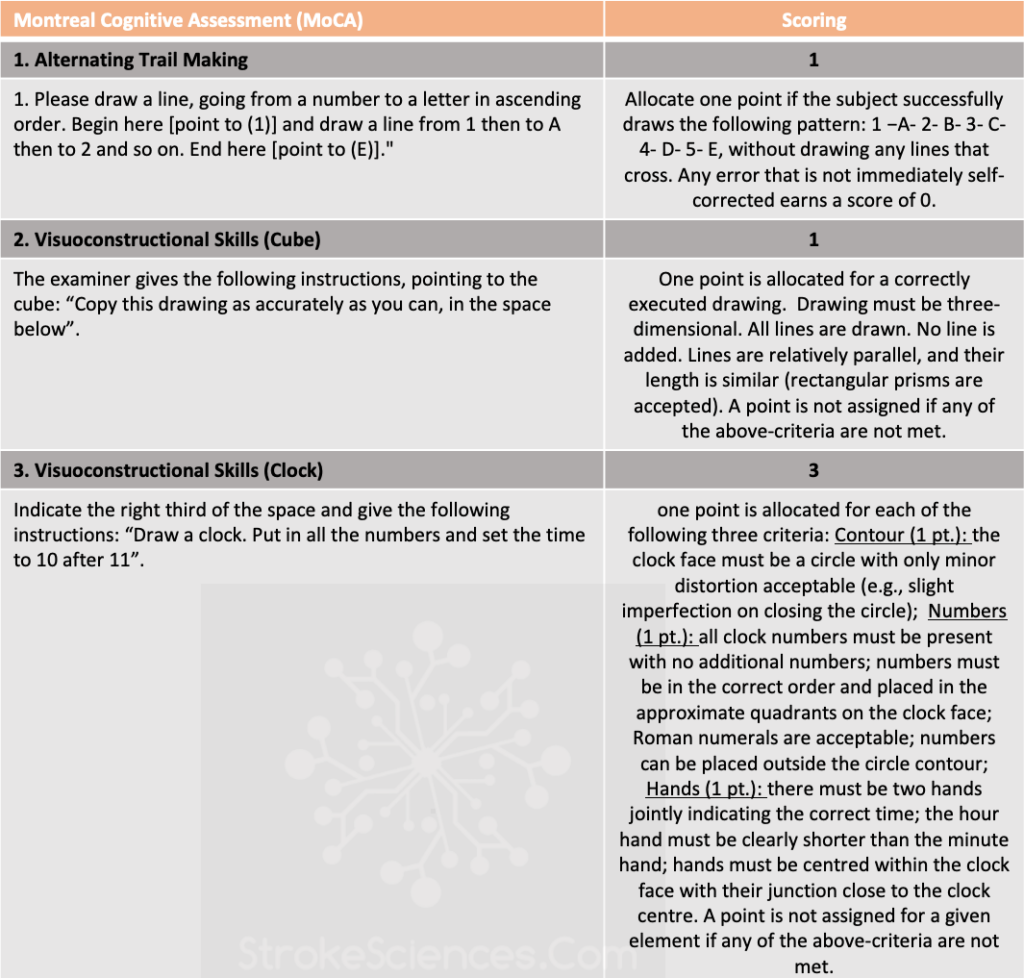
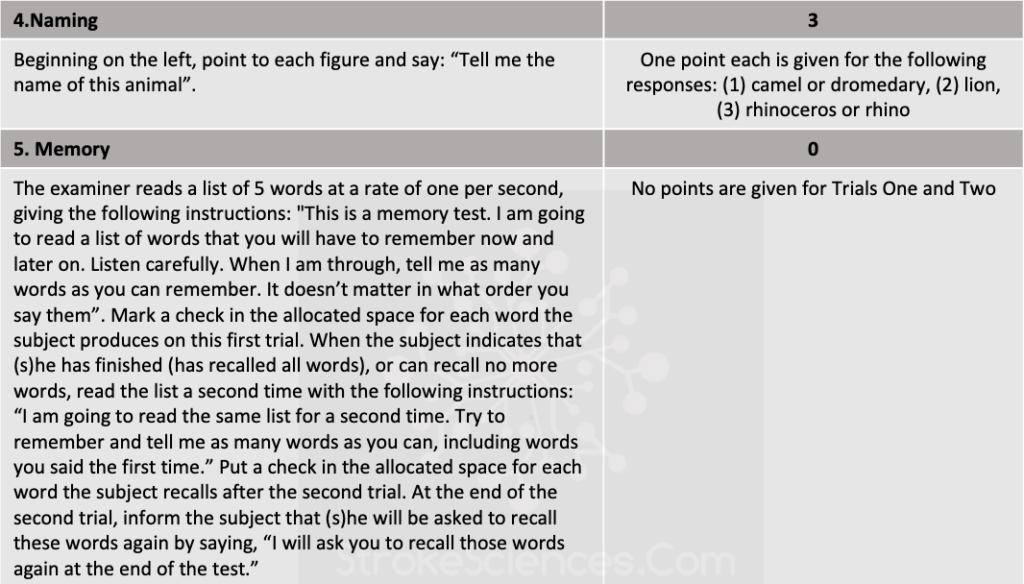
- 3- Montreal Cognitive Assessment (MoCA): Sensitivity, Specificity and Predictive Values
- 4- MMSE and MoCA forms to download (PDF- English & French)
- 5- References
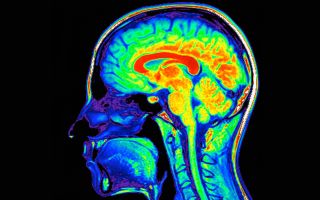
1-Introduction
Whether hemorrhagic or ischemic, stroke is the main cause of vascular cognitive impairment (VCI). From executive function to memory, attention and motor planning, cognitive ability of a patient is a strong determinant of longterm outcome and prognosis. Given the fact that in our modern medicine each patient is assessed and treated by multiple clinicians developing clinical tests deemed necessary. This makes sense. When a patient is seen by a neurologist or a physiatrist it is easier to look at the chart and see a test score assigned to the patient by previous clinicians. This approach tends to stratify patients based on their scores and makes it easier to follow the progression of disease or in some cases efficacy of treatments and therapeutics.
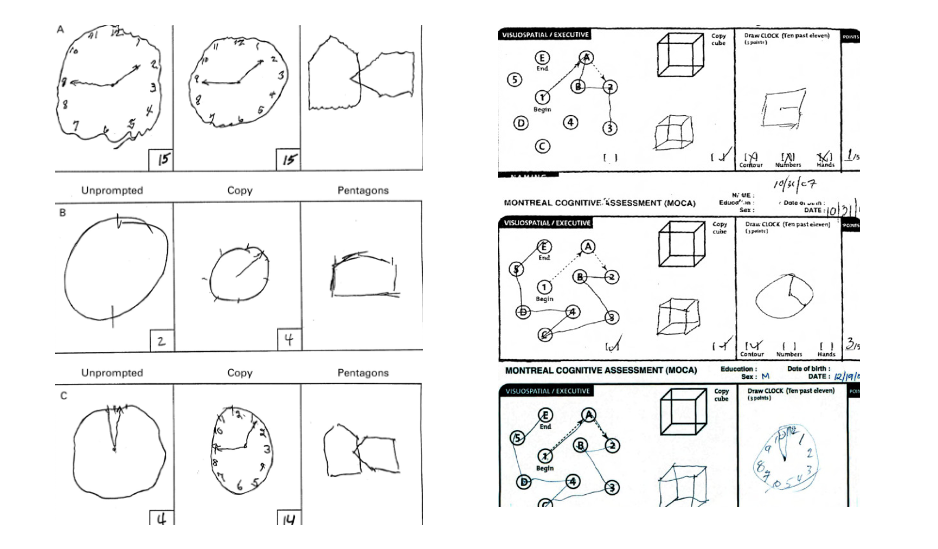
However, such approaches expose clinicians to bias and misinterpretation. Despite training and certification in administering these tests Inter-rater reliability is one of the major treats, especially when there is a cutoff to determine if a patient is or is not cognitively competent. Based on my observations, many patients are labeled unworthy of rehab after stroke and sent to longterm care institutions because of a MoCA test that was administered 3 days after stroke. We all are familiar with the post-stroke inflammatory processes and network reorganization that occur within the first few months after stroke. Most stroke patients have much higher cognitive scores few weeks after the onset. This issue begs the following questions: Do we have appropriate institutional guidelines for the timeline of administration of such tests? when should cognitive tests be administered?
We ought to realize that these scores are stored in patients medical records and are highly consequential parameters in the course of patients journey to treatment and recovery. Just like an IQ score that can change the course of a child’s life or a credit score that can affect a family’s livelihood a cognitive score specifically in stroke population can directly affect the course of recovery or the choice of rehab institutions. It is therefore important to consider factors such as inter-rater reliability which evaluates the consensus amongst clinicians to score patients in a similar fashion, and test-retest reliability which measures the consistency of the test over time as well as sensitivity and specificity of such tests before assign cutoff scores as requirement for admission and discharge. In the following sections using an evidence-based approach we explore important features of MMSE and MoCA and their significance in clinical and research settings.
2- Mini-Mental Status Examination (MMSE)
The MMSE was introduced by Folstein in 1975 as an 11-part bedside test requiring only 5-10 minutes to administer, a much briefer time compared with the 1-2 hour long formal tests for dementia (Gluhm et al., 2013). While the MMSE was originally developed to screen for dementia and delirium, many neurologists use this measure as a screening instrument for ‘cognitive impairment’ in hospitalized stroke patients (Nys et al., 2005). Assuming there is no evidence of delirium, a MMSE score of 23 or less increases the probability of dementia greatly, whereas a score of 24-30 decreases it. Nonetheless, because false-positive results become a concern when applying this threshold to large populations with a low incidence of dementia, such as persons living independently in community, some experts prefer interpreting the MMSE score in three ranges (Dick et al., 1984; Kahle-Wrobleski et al., 2007). In general it is not easy to determine a universal cutoff score due to cultural, socioeconomic and education background of each patient in one region let alone in different countries (Kochhann et al., 2010). However, MMSE in North America score of 20 or less rules in dementia, 21-25 is regarded as less conclusive prompting further investigation, and 26 or more rules out dementia (Kochhann et al., 2010; Nys et al., 2005; Tsai et al., 2016).
3- Montreal Cognitive Assessment (MoCA)
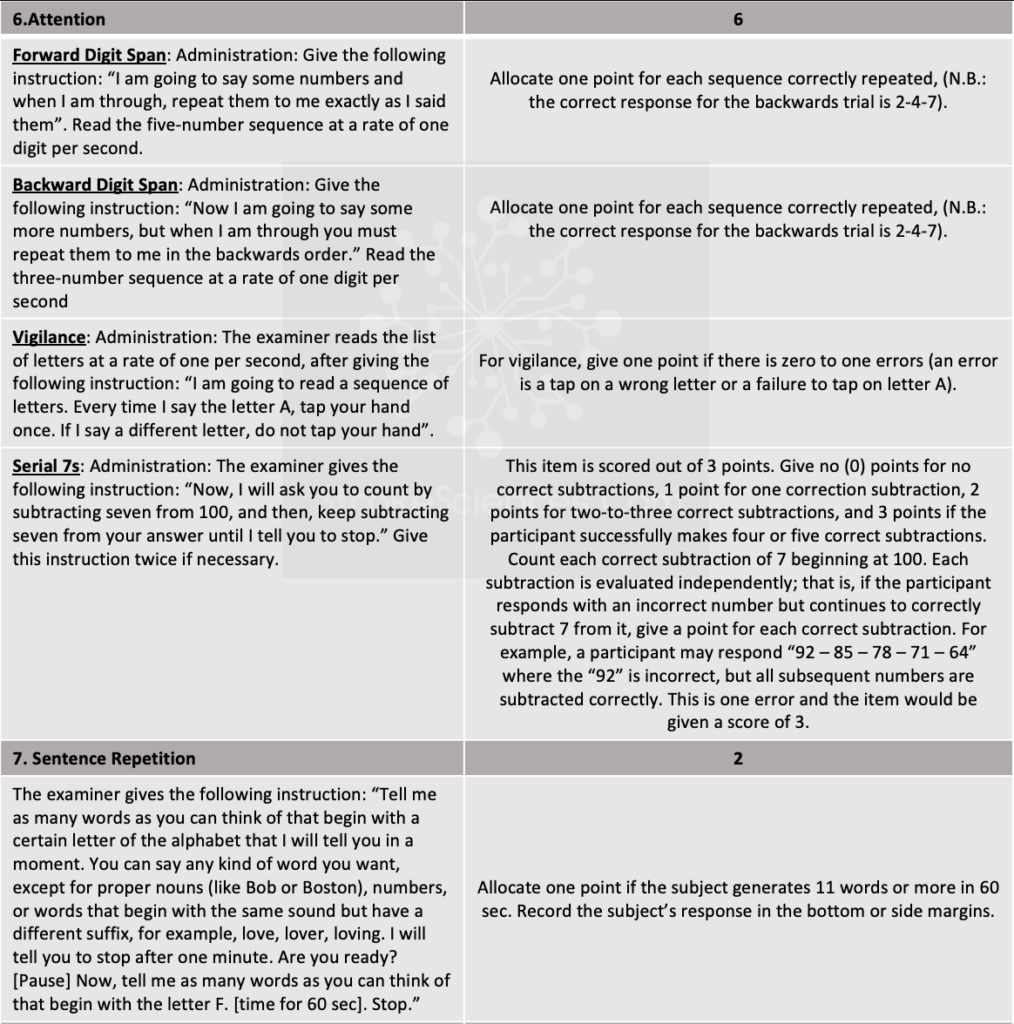
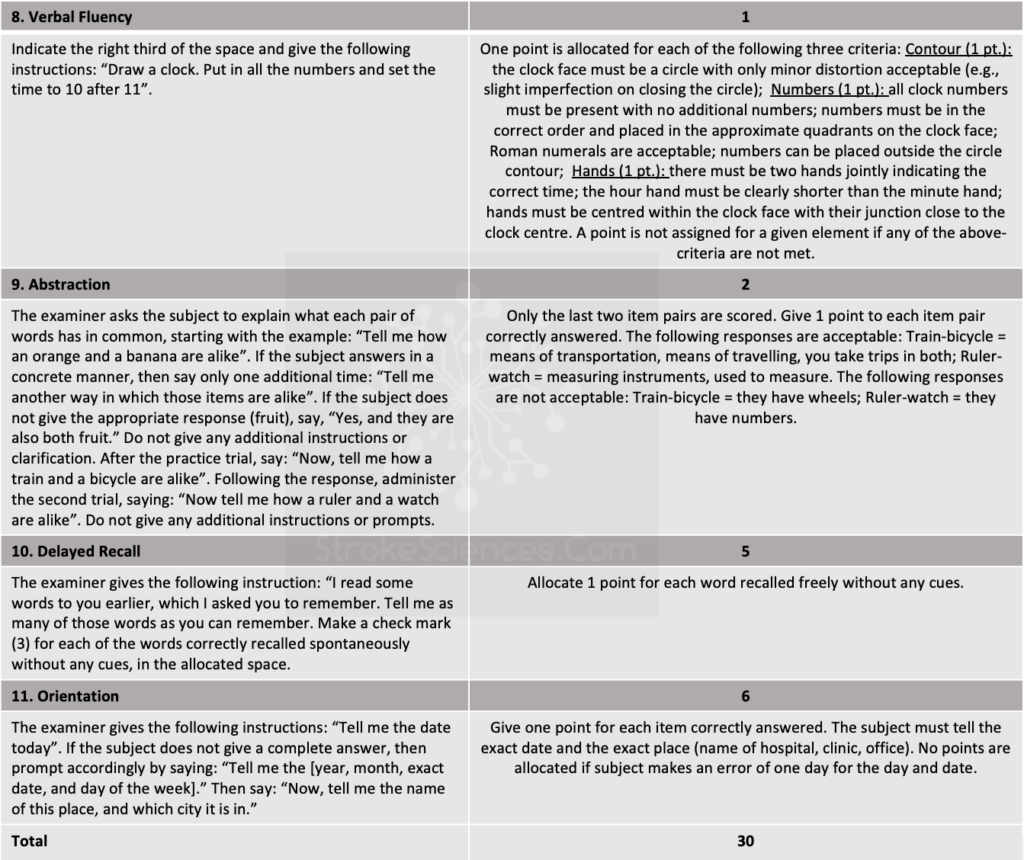
The neuropsychological assessment of patients with suspected VCI requires a comprehensive battery, which should include tests sensitive to executive function abnormalities, as a feature of the condition. Thus, in recent years MoCA has been recommended, stadardized and referenced in NINDS-CSN guidlinesin place of MMSE because the former is more sensitive for the detection of executive function abnormalities (Xu et al., 2016). MoCA is a brief screening instrument originally designed to identify MCI in elderly patients attending a memory clinic. It is a one page, 30-point test, that can be administered in approximately 10 minutes (Thomann et al., n.d.). MoCA evaluates different domains: visuospatial abilities, executive functions, short-term memory recall, attention, concentration, working memory, language, and orientation to time and space. Although MoCA is a great tool to examine the cognitive function, deficits in executive function are not always specific c to cerebrovascular disease. In a study of Framingham Heart Study subjects comparing new cognitive deficits that appeared in persons after stroke with cognitive deficits appearing over time in persons without stroke (Weinstein et al., 2014). Despite such downfalls, studying 493 patients, Pendlebury and colleagues (2010) concluded that the MoCA picked up substantially more cognitive abnormalities after transient ischemic attack and stroke than the MMSE, demonstrating deficits in executive function, attention, and delayed recall (Pendlebury Sarah T. et al., 2010).
4- MMSE and MoCA forms to download (PDF- English & French)
Download MMSE-PDF (English & French)
 Loading…
Loading…
 Loading…
Loading…
Download MoCA-PDF (English & French)
 Loading…
Loading…
 Loading…
Loading…
5- References
Chiti Guido, & Pantoni Leonardo. (2014). Use of Montreal Cognitive Assessment in Patients With Stroke. Stroke, 45(10), 3135–3140. https://doi.org/10.1161/STROKEAHA.114.004590
Ciesielska, N., Sokołowski, R., Mazur, E., Podhorecka, M., Polak-Szabela, A., & Kędziora-Kornatowska, K. (2016). Is the Montreal Cognitive Assessment (MoCA) test better suited than the Mini-Mental State Examination (MMSE) in mild cognitive impairment (MCI) detection among people aged over 60? Meta-analysis. Psychiatria Polska, 50(5), 1039–1052. https://doi.org/10.12740/PP/45368
Cooley, S. A., Heaps, J. M., Bolzenius, J. D., Salminen, L. E., Baker, L. M., Scott, S. E., & Paul, R. H. (2015). Longitudinal change in performance on the Montreal Cognitive Assessment in older adults. The Clinical Neuropsychologist, 29(6), 824–835. https://doi.org/10.1080/13854046.2015.1087596
Cummings-Vaughn, L. A., Chavakula, N. N., Malmstrom, T. K., Tumosa, N., Morley, J. E., & Cruz-Oliver, D. M. (2014). Veterans Affairs Saint Louis University Mental Status examination compared with the Montreal Cognitive Assessment and the Short Test of Mental Status. Journal of the American Geriatrics Society, 62(7), 1341–1346. https://doi.org/10.1111/jgs.12874
Dick, J. P., Guiloff, R. J., Stewart, A., Blackstock, J., Bielawska, C., Paul, E. A., & Marsden, C. D. (1984). Mini-mental state examination in neurological patients. Journal of Neurology, Neurosurgery, and Psychiatry, 47(5), 496–499. https://doi.org/10.1136/jnnp.47.5.496
Dong, Y., Lee, W. Y., Basri, N. A., Collinson, S. L., Merchant, R. A., Venketasubramanian, N., & Chen, C. L.-H. (2012). The Montreal Cognitive Assessment is superior to the Mini-Mental State Examination in detecting patients at higher risk of dementia. International Psychogeriatrics, 24(11), 1749–1755. https://doi.org/10.1017/S1041610212001068
Gluhm, S., Goldstein, J., Loc, K., Colt, A., Van Liew, C., & Corey-Bloom, J. (2013). Cognitive Performance on the Mini-Mental State Examination and the Montreal Cognitive Assessment Across the Healthy Adult Lifespan. Cognitive and Behavioral Neurology : Official Journal of the Society for Behavioral and Cognitive Neurology, 26(1), 1–5. https://doi.org/10.1097/WNN.0b013e31828b7d26
Gupta, M., Gupta, V., Nagar Buckshee, R., & Sharma, V. (2019). Validity and reliability of hindi translated version of Montreal cognitive assessment in older adults. Asian Journal of Psychiatry, 45, 125–128. https://doi.org/10.1016/j.ajp.2019.09.022
Kahle-Wrobleski, K., Corrada, M. M., Li, B., & Kawas, C. H. (2007). Sensitivity and specificity of the mini-mental state examination for identifying dementia in the oldest-old: The 90+ study. Journal of the American Geriatrics Society, 55(2), 284–289. https://doi.org/10.1111/j.1532-5415.2007.01049.x
Kochhann, R., Varela, J. S., Lisboa, C. S. de M., & Chaves, M. L. F. (2010). The Mini Mental State Examination: Review of cutoff points adjusted for schooling in a large Southern Brazilian sample. Dementia & Neuropsychologia, 4(1), 35–41. https://doi.org/10.1590/S1980-57642010DN40100006
Koski, L. (2013). Validity and Applications of the Montreal Cognitive Assessment for the Assessment of Vascular Cognitive Impairment. Cerebrovascular Diseases, 36(1), 6–18. https://doi.org/10.1159/000352051
Nys, G. M. S., van Zandvoort, M. J. E., de Kort, P. L. M., Jansen, B. P. W., Kappelle, L. J., & de Haan, E. H. F. (2005). Restrictions of the Mini-Mental State Examination in acute stroke. Archives of Clinical Neuropsychology, 20(5), 623–629. https://doi.org/10.1016/j.acn.2005.04.001
Pendlebury Sarah T., Cuthbertson Fiona C., Welch Sarah J.V., Mehta Ziyah, & Rothwell Peter M. (2010). Underestimation of Cognitive Impairment by Mini-Mental State Examination Versus the Montreal Cognitive Assessment in Patients With Transient Ischemic Attack and Stroke. Stroke, 41(6), 1290–1293. https://doi.org/10.1161/STROKEAHA.110.579888
Potocnik, J., Ovcar Stante, K., & Rakusa, M. (2020). The validity of the Montreal cognitive assessment (MoCA) for the screening of vascular cognitive impairment after ischemic stroke. Acta Neurologica Belgica, 120(3), 681–685. https://doi.org/10.1007/s13760-020-01330-5
Simmons, B. B., Hartmann, B., & DeJoseph, D. (2011). Evaluation of Suspected Dementia. American Family Physician, 84(8), 895–902. Tan, J., Li, N., Gao, J., Wang, L., Zhao, Y., Yu, B., Du, W., Zhang, W., Cui, L., Wang, Q., Li, J., Yang, J., Yu, J., Xia, X., & Zhou, P. (2015). Optimal cutoff scores for dementia and mild cognitive impairment of the Montreal Cognitive Assessment among elderly and oldest-old Chinese population. Journal of Alzheimer’s Disease: JAD, 43(4), 1403–1412. https://doi.org/10.3233/JAD-141278
Thomann, A. E., Goettel, N., Monsch, R. J., Berres, M., Jahn, T., Steiner, L. A., & Monsch, A. U. (n.d.). The Montreal Cognitive Assessment: Normative Data from a German-Speaking Cohort and Comparison with International Normative Samples. Journal of Alzheimer’s Disease, 64(2), 643–655. https://doi.org/10.3233/JAD-180080
Tsai, J.-C., Chen, C.-W., Chu, H., Yang, H.-L., Chung, M.-H., Liao, Y.-M., & Chou, K.-R. (2016). Comparing the Sensitivity, Specificity, and Predictive Values of the Montreal Cognitive Assessment and Mini-Mental State Examination When Screening People for Mild Cognitive Impairment and Dementia in Chinese Population. Archives of Psychiatric Nursing, 30(4), 486–491. https://doi.org/10.1016/j.apnu.2016.01.015
Tu, Q., Jin, H., Ding, B., Yang, X., Lei, Z., Bai, S., Zhang, Y., & Tang, X. (2013). Reliability, Validity, and Optimal Cutoff Score of the Montreal Cognitive Assessment (Changsha Version) in Ischemic Cerebrovascular Disease Patients of Hunan Province, China. Dementia and Geriatric Cognitive Disorders EXTRA, 3(1), 25–36. https://doi.org/10.1159/000346845
Weinstein, G., Preis, S. R., Beiser, A. S., Au, R., Kelly-Hayes, M., Kase, C. S., Wolf, P. A., & Seshadri, S. (2014). Cognitive performance after stroke—The Framingham Heart Study. International Journal of Stroke: Official Journal of the International Stroke Society, 9 Suppl A100, 48–54. https://doi.org/10.1111/ijs.12275
Wong, A., Yiu, S., Nasreddine, Z., Leung, K., Lau, A., Soo, Y. O. Y., Wong, L. K., & Mok, V. (2018). Validity and reliability of two alternate versions of the Montreal Cognitive Assessment (Hong Kong version) for screening of Mild Neurocognitive Disorder. PLOS ONE, 13(5), e0196344. https://doi.org/10.1371/journal.pone.0196344
Xu, X., Chan, Q. L., Hilal, S., Ikram, M. K., Venketasubramanian, N., Tan, B. Y., Dong, Y., Chen, C. L.-H., & Collinson, S. L. (2016). The Diagnostic Utility of the NINDS-CSN Neuropsychological Battery in Memory Clinics. Dementia and Geriatric Cognitive Disorders EXTRA, 6(2), 276–282. https://doi.org/10.1159/000445050